The cardiovascular regulatory system is made up of a number of feedback loops, working together to maintain homeostasis. Their job is to keep blood flowing at the right volume, speed and consistency to keep all our tissues fed with nutrients, supplied with oxygen and free of toxins.
In the next Arsenic Files we will be looking at the cardiovascular regulatory system particularly the Renin-Angiotensin-System (RAS), Bradykinin, which is part of the Kallikrein-Kinin-System (KKS) and other components that feed in to the regulatory system. We hope to find out, through looking at these in detail and how they may interact with arsenic, whether ACE2 really is the culprit.
Renin-agiotensin-system (RAS)
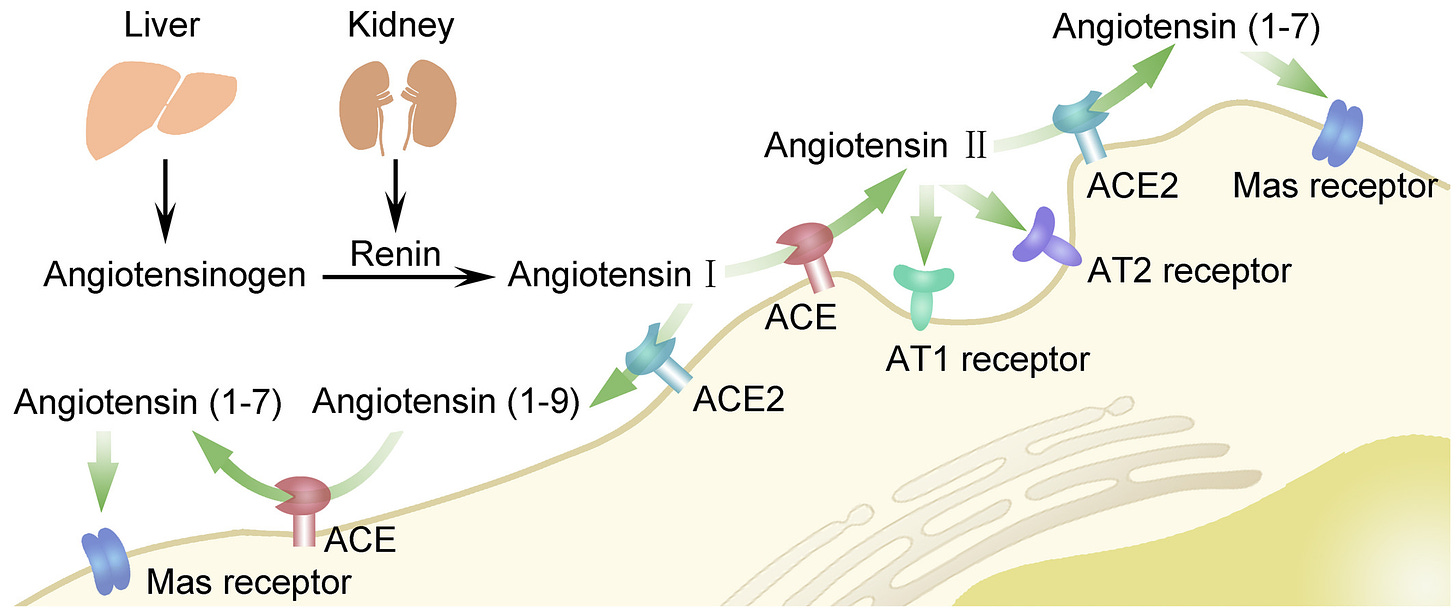
RAS controls blood volume and vascular resistance. It protects us from low blood pressure by calibrating the balance of two key electrolytes, sodium and potassium. Here is a quick summary together with a very helpful explanatory diagram.
The juxta-glomerula cells continually produce prorenin which circulates around the body. When the environment in the kidneys and blood is acidic, prorenin converts to renin. That acidic environment is created by the production of reactive oxygen species (ROS), a result of cellular injury . Read this article for production of ROS by Arsine gas molecules. The tissue injury that creates ROS also precipitates electrolyte and fluid loss resulting in a drop in blood pressure.
This drop in pressure is sensed by baroreceptors in the carotid sinus (neck) and the juxtaglomerula cells (kidneys). The affrent and effrent (in and out) vessels in the kidneys sense if pressure and sodium levels are dropping. Sympathetic nervous system Beta 1 adrenergic receptors in the heart, cerebral cortex and kidneys also sense the drop in blood pressure.
In addition to the RAS response to signalling, vasopressin is produced in the hypothalamus after receiving a signal from baroreceptors.
The liver constantly produces a compound called Angiotensinogen. This circulates in the body ready to be called in to action. When Renin molecules are activated they join to Angiotensinogen peptide chains distributed around the body. Renin then cleaves (disconnects) the first 10 peptides from the rest of the chain. The new shorter peptide chain is called Angiotensin I (Ang I).
The first pathway - ACE to ACE2
There are two key pathways that Ang I can now take. In the first it can be converted by ACE in to Angiotensin II (Ang II), which can then attach to AT1 and AT2 receptors in the cell. ACE is highly expressed in the lungs, the gut, kidney, bladder, male and female sexual organs.
AT1 receptor works to regulate blood pressure by controlling electrolyte and water balance, hormones and kidney function. If blood pressure is low, this receptor can help raise blood pressure.