Neurodegenerative diseases are on the rise. The National Institute of Environmental Health Services states that there are approximately 6.2 million people living with Alzheimers and nearly 1 million with a Parkinson’s diagnosis. In the UK, 2019, over 850,000 people were said to have a dementia/Alzheimers diagnosis (Alzheimer’s Society) and 145,000 a Parkinson’s diagnosis by 2018 (Parkinson’s UK). Levels are predicted to climb.
This study on ageing concludes that as the population ages we are to expect increasing levels of neurodegeneration. Authors summarise the contributing factors as age related ‘genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, mitochondrial dysfunction, cellular senescence, deregulated nutrient sensing, stem cell exhaustion and altered intercellular communication’. In plain english a general break down in cell function and correct replication of cells and proteins. It seems a reasonable list but there are issues.
Why do only 1 in 9 American people develop Alzheimers? What about the rest of the aging population? If brain degeneration were a natural part of aging would we not expect to see everyone over the age of 65 developing one or other neurological disease? Instead some people succumb to cardiovascular disease, others liver and kidney issues, and others arthritis. Many live to a ripe old age with hardly an ailment.

In this article we focus on Alzheimers, Parkinsons, Creutzfeldt Jakob and Motor Neurone (ALS) diseases with some mentions of other neurological conditions. We will look at markers in the blood and cerebro spinal fluid, and how arsenic and other toxins can affect cell function, iron build up and protein formation.
Iron
Iron seems to play a central role in both autoimmune and neurodegenerative disease. Iron overload causes oxidative damage (ROS) and general toxicity to the cells. In Alzheimers, brain inflammation occurs with uptake of non-transferrin-bound iron (NTBI) by the brain ventricular system, liver and kidneys. Marked increases in ferritin, a protein that regulates circulating iron levels, coupled with a reduction in haemoglobin have also been observed.
Ferritin is an indicator of inflammation in the body from pathogens or injury. Inflammation only ever happens in response to injury either on a micro or macro level – burst red blood cells or a broken leg. The level of inflammation gives us an idea of how widespread cell death is, as do ferritin levels.
Ferritin is an insoluble form of iron, and not bioavailable. This would then explain why anemia, as well as iron overload, can be seen in patients with Alzheimers. Anemia was found to be 19% higher in this study of patients with Alzheimers and dementia related diseases. Reinhold Schmidt, in a European led study, found that significant iron deposits were found in deep grey matter, neocortex, temporal and occipital lobes.
It was also noted as disease progressed, that iron continued to accumulate in these areas of the brain. However, the researchers were unable to conclude if the disregulation of iron itself was causing the issues, or if it was just a marker corresponding to cognitive decline.
In this paper looking at Ferritin, iron and Complex 1 in Parkinson’s disease, the substantia nigra area of the brain, the focal point for Parkinson’s, showed marked increase in iron levels, with associated oxidative damage Complex 1 is a large protein in the mitochondria which enables transfer of electrons to create energy. In the substantia nigra this protein is markedly reduced, meaning energy production and other functions carried out by the mitochondria, including heme synthesis, intercellular messaging and regulation of cell death are all impaired in these brain cells.
Again, similarly to Alzheimers and Huntingdon’s (a genetic disease), an increase in total brain iron presents in Creutzfeldt Jakob disease, together with a functional iron deficiency. Transferrin levels, proteins that bind iron and other metals in the blood for transportation, and transferrin receptors increase as the disease progresses, whilst insoluble and non-bioavailable ferritin bound iron in the cells increases uncontrollably, leading to oxidative damage and cell death.
The study identified the affinity iron has with the PrPc protein, of which the mutated form PrP(sc) serves as an indicator of CJD. Researchers, however, struggled to determine what role iron had in the formation of these mutated ‘prion’ proteins. Did the iron imbalance cause the misfolded protein, or the misfolded protein cause the iron imbalance, or are the two equally affected by something else? They concluded that the prion infection created iron imbalance, that iron deficiency was apparent early on in the disease, and was likely a result of prion mutation.
Motor Neurone disease or amyotrophic lateral sclerosis (ALS) is a disease characterised by the loss of voluntary control of muscles in the body via the primary motor cortex, an area in the top anterior part of the brain. Again raised ferritin was detected as was transferrin. Ferritin levels in the cerebro spinal fluid and iron overload in the brain increased as the illness progressed, whereas there seemed to be no correlation between progression and transferrin levels. There was also an increase in Hemoglobin A1c levels, conversely to Alzheimer’s patients who saw a reduction.
In all five diseases there seems to be a marked increase in ferritin, with anemia in four. Iron overload in the brain is a strong marker for neurodegeneration.
Copper and Zinc
Copper is a transition metal. It is crucial for iron metabolism, conversion of neurotransmitters dopamine in to norepinephrine, and energy production. In our review, copper (II) was found to enhance abnormal protein formation in both Alzheimers and Parkinson’s disease. Blood levels of copper (serum) and copper transporting protein, Ceruloplasmin were both raised in Alzheimer’s but were stable in Parkinson’s. There was a marked decrease in copper but an increase in zinc in the substantia nigra brain area in Parkinsons. The copper levels in the cerebro spinal fluid (CSF) were much increased.
Zinc is used in cellular metabolism and mytosis (cell division), multiple enzyme processes, immunity, protein and DNA synthesis, and wound healing. It has been associated with an additional fold in the CJD prion PrPc due to changes in charge on the protein surface. The changes seem to weaken existing zinc bonds and allow the potential misfolding of the protein in to the prion disease form PrP(sc). Both free copper and zinc appeared to increase the chances of misfolding proteins in a laboratory setting (in-vitro).
Interestingly histidine, an essential amino-acid for protein production (not made by the human body), can chelate (bind) metal ions. Histidine was found to prevent zinc from blocking absorption of copper in the intestine, binding with copper to make it more bioavailable. Copper(II)-L-Histidine complex has been used in children with Menkes disease, a condition where copper transport is impaired (from in-utero onwards) and can lead to early death. It has also been used as a therapy for Wilson’s disease, an inherited disease which leads to build up of copper in the kidneys.
In CJD, research has found that healthy PrPc proteins binds copper, and play a role in controlling oxidative status in the brain. D. R. Brown at the University of Cambridge found that it seemed to have an antioxidant role which required copper to function. The N-terminus of the protein binds tightly to copper and less tightly to other metals. If manganese for example takes over the copper position, the protein becomes resistant to proteases (a chemical which speeds up protein breakdown). Scrapie type symptoms were induced in mice who were treated with a copper chelator, suggesting that the loss of copper from the PrPc protein may play a part in the misfolding process. What displaces it?
Trafficking arsenic
Brain and Cell Access
Before arsenic can create havoc in the brain it has to get past the highly discrimatory blood brain barrier. Each capillary in the brain is made up of very tightly packed cells (tight junctions) that act as a filter. Oxygen, small fat soluble molecules and glucose can cross the barrier between capillaries and brain cells. Drugs for epilepsy, schizophrenia, caffeine, alcohol can also make it across the barrier. Surface molecules (receptors) on endothelial cells pick up required nutrients and push them through to the other side of the endothelium in to the brain. There are also efflux pumps, similar to what we see in bacteria, which push out any unwanted molecules.
To get across this barrier either a particle needs to piggy back on the back of a molecule that is readily accepted by the receptors, or it needs to affect the proteins that control the tight junctions (similar to tight junctions in the lungs and gut). Exposure of the capillary wall to arsenic in mice led to the decrease in mRNA expression for tight junction proteins, causing permeability and allowing arsenic to cross over the blood brain barrier.
Cell access
Inorganic Arsenite (III), the anerobic form of arsenic, uses the channels GLUT1 and APQ9. GLUT1 is Glucose Transporter 1, which, as the name suggests, transports glucose across cell membranes. GLUT1 encodes the main glucose transporter across the blood brain barrier (BBB) as well as covering 2% of the membrane of erythrocytes (normal cells). Arsenite is a much smaller molecule than glucose so takes advantage of this channel to enter the cells.
Aquaporin 9 is an even more interesting channel of access. It is a two way channel in a series of aquaporins largely dedicated to the swift transfer of water in and out of the cell. This particular channel allows glycerol in and out of the cell. As well as being used to maintain osmotic pressure in the brain, glycerol is believed to act as part of glycerol-3-phosphate as a shuttle in to the mitochondria in order to aid energy production through glycolisis. Arsenite, being of a similar size to glycerol, easily mimicks the molecule and gains easy access through these virtually open channels in to the cells.
Inorganic Arsenate (V), the aerobic form of arsenic, mimicks the structure of phosphate and uses the phosphate transporters in the cell. Phosphate is part of energy production, cell membrane structure and DNA. We have already talked about how the invasion of arsenic species in to the cells interrupts the energy cycle through displacement of phosphate here.
In an ideal world arsenic species endering the cells would be methylated and make a swift exit via multidrug resistant proteins. However, the affinity arsenite and arsenate have with specific elements means that they can cause a whirlwind of disruption and potentially even hijack the cells permanently leading potentially to oncogenic growth.
As we know from previous research, arsenic species have a high affinity with sulphur-containing cysteine residues and sulphydryl groups, and can create a particularly strong bond with disulphide groups (two sulphur molecules). Mercury, lead and cadmium are examples of other toxic metals that have an affinity with sulphur. We have talked about zinc finger anchors in the transmembrane proteins of the cell nucleus, and how arsenic can influence functions, including reactivation of the Sonic Hedgehog pathway, which promotes embryonic speed of growth. Arsenic can also adhere to iron-sulphur clusters within cells, releasing free iron and causing widespread oxidation through the Fenton Reaction. This would damage other molecules, releasing more iron and other metals.
Self destruct button off
Cell senescence is usually a response to ‘oncogenic activation, oxidative and genotoxic stress, mitochondrial dysfunction, irradiation, or chemotherapeutic agents’. In order for cells to die, the BAX protein must activate the process. BAX is located in the cystosol (outside of the nucleus and mitochondria) of a cell. Arsenic trioxide, one species of the group of arsenic molecules, is able to alter the way BAX works, binding it via cysteine molecules to the anti-apoptosis (cell death) protein Bcl-XL, which sits in the wall of the mitochondria.
Bcl-XL prevents the release of Cytochrome C molecules from the mitochondria, which signal to the cell that it needs to die. Cytochrome C molecules are iron containing. When a cell is at the end of its life Cytochrome C migrates from the mitochondria in to the cytosol. The binding by arsenic of the pro-apoptosis protein BAX to the anti-apoptosis protein Bcl-XL draws BAX in to the mitochondria, preventing cell death. This is how cells can remain active in an altered and pro-oncogenic state (cancer forming). https://www.sciencedirect.com/topics/medicine-and-dentistry/bcl-xl. Even more interestingly reactive oxygen species (ROS), the element that is said to cause so much damage to cells, can actually block this action, allowing cells to die in a timely manner.
Frataxin
Along with the retention of iron-containing cytochrome C in the mitochondria in Bcl-XL/BAX affected cells, the sulphur-iron synthesising protein Frataxin may also contribute to systemic overload of iron in the malfunctioning cells. It seems to have a regulatory function in the cell, synthesising iron-sulphur clusters when needed, and also regulates iron transfer. Failure of the frataxin protein leads to iron build up in the mitochondria. Friedreich’s ataxia, a genetic disease, develops as a result of the failure of this protein. The cysteine molecules in frataxin, required to enable iron-sulphur cluster synthesis, are of course targets for arsenic, which would inevitably alter their function detrimentally.
Protein folding and clumping
The neurodegenerative diseases we have been looking at all have one thing in common. They all exhibit some degree of protein interference. Some proteins will clump together creating a signal blocking structure such as Amyloid Beta in Alzheimers. Other proteins will misfold such as PrPc in to PrP(sc) in CJD. Let’s have a look at how that could happen.
Amyloid beta peptide
Amyloid beta chains are peptides, or strings of amino acids which are the building blocks of proteins. This study showed interference by arsenic metabolite dimethylarsinic acid (DMA), in the processing of amyloid precursor protein.
The amyloid precursor protein (APP) is cysteine (sulphur-containing molecule) rich and also contains three disulphide bridges. These two sulphur molecule bridges connect the folds that maintain its structure. Arsenic can attach to these disulphid bridges as well as to other cysteine molecules in the peptide. Copper is also present, which we know can also be displaced by arsenic. This interference alters the metabolite of APP, creating the defective amyloid beta peptides that we see in Alzheimers.
There are two hypotheses, that change in the gene that regulates APP formation, creates the mutated amyloid beta, or that it is a functional change in the APP itself that causes the mutation. It is also possible that arsenic also influences sulphur containing amino acids in mRNA and RNA leading to incorrect transcription.
B-amyloid mutations and clumps can be found in a number of neurodegenerative illnesses including Alzheimers, Parkinson’s, CJD (spinal fluid), Huntingtons and Niemann-Pick type C or Pick’s disease.
Tau Tangles
Tau proteins are also targets for arsenic species. The group of proteins can be hyperphosphorylated by Arsenic, creating Tau Tangles. Tau proteins maintain the structure of axon microtubules and are abundant in the central nervous system. They are quite like the fibres in fibreoptic broadband. The tangles created by the presence of arsenic effectively cause physical blocks in signalling. Tau tangles or tauopathies are found not only in Alzheimer but in Parkinson’s, CJD, ALS, Huntingdons, progressive supranuclear palsy, Pick's disease and corticobasal degeneration. Undoubtedly they would be found in many neurodegenerative diseases.
Arsenite and Cadmium adhesion to αSyn
In Parkinsons α-Synuclein is the proposed problem presynaptic neuronal protein. It is thought that its formation of protofibrils, is the cause cellular disruption, and that the secretion of the αSyn protein is damaging to other cells. α-Synuclein regulates synaptic messaging and is abundant in the brain, with smaller amounts in the heart, muscle and other tissues. The formation of normal fibres begins with the creation of oligomers out of αSyn monomers. These then grow in to longer lengths called amyloid fibres, forming the vehicle for synaptic messaging.
In vitro experiments show that both Cadmium (II) and Arsenite (III) can prevent refolding of proteins by attaching to metal binding sites. There are three metal binding areas in the protein αSyn, the N-terminus, the histidine at position 50 (H50), and C-terminal residues. In this experiment the H50 and C-terminals are both potential binding sites for these two elements.
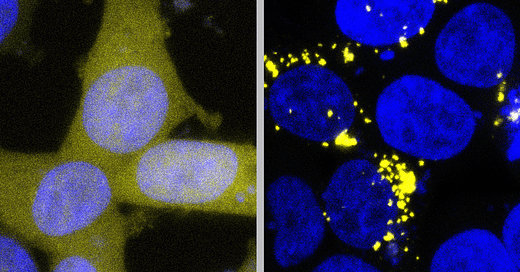
Importantly it has been shown that proteins triggered by both cadmium and arsenite seem to be able to create ‘seeds that, in a gain-of-function mechanism, increased the misfolding and aggregation of other proteins’. It could be that the ‘seeds’ are infact arsenic or cadmium transferring from protein to protein, or that there is just a plentiful supply. In this experiment the new fibers took up 50% of the metal from the solution in vitro giving a 1:2 metal to monomer ratio, meaning there is plenty of metal to communicate to other proteins. When dyed with a green flourescent protein, the presence of arsenic and cadmium cause usually evenly spaced αSyn molecules to clump. When the metal content in-vitro was increase, the clumping also increased.
PrP protein misfold to PrP(sc)
Arsenic, lead, cadmium and mercury have an affinity with sulphur molecules in proteins. Whilst we are unable to find any papers on the relationship between CJD and arsenic, we did find a paper on a case of mercury poisoning that presented with Parkinsonian symptoms which was attributed to CJD. The write up on the case of the 42 year old patient suggests that clinicians should consider mercury poisoning in those presenting with sporadic CJD symptoms. This suggests that a similar effect from arsenic should also be possible.
In any process requiring reconfiguration of proteins, proteins must first unfold and then refold when reorganisation is complete. This is where BAX (as seen in the regulation of iron in cells) comes in. PrP seems to be cytoprotective, preventing BAX from triggering cell death. BAX also has an effect on the unfolding protein response. It, together with Bak, prevents early protein unfolding in the face of stressors. When arsenic joins BAX to the Bcl-XL protein, BAX essentially becomes disabled. The proteins are then free to unfold. It is possible that arsenic also then anchors to the disulphide bridge at Cys214 and Cys179 which keeps the protein in this PrP(sc) position that leads to the illness known as CJD, instead of adopting the correct PrPc position.
Prion disease, or the misfolding of proteins is also suspected in Parkinson’s. Research suggests that ‘misfolded alpha synuclein protein filaments and aggregates’ can transfer to other nearby cells, which is how CJD spreads in the brain. Huntingtons is also shown to be a prion disease (familial). New findings in a review in February 2019 also found Alzheimers (Tau and Amyloid beta) to have features of prion disease.
Summary
There is a lot to take in in this article. The key findings are that neurodegenerative diseases all seem to involve derangement of iron, copper and zinc, which can be caused by Arsenic through the mechanisms detailed. Arsenic gains access through the blood brain barrier by altering sulphur containing molecules, mimicking other molecules, and continuing to cause protracted damage.
Some diseases appear to be one type of neurodegeneration and are then labelled something else. Patients may be diagnosed with two or more concurrent neurodegenerative diseases, as in this Alzheimer’s case, also presenting with a change in motor function.
In the process of degeneration, each neurological disease manifests according to the main area of the brain exposed and, as we see in CJD, speed of degeneration. Could this variability be down to levels and rate of exposure to arsenic, or other neurotoxic metals? Is there evidence to suggest a link between arsenic exposure and neurodegenerative disease? Yes, we think there is.
What we are not sure of yet is why certain people are more susceptible than others. There seems to be some link to physical build. Slender people seem more affected than those who are overweight, though that does not preclude the latter group. Arsenic can be detoxified via the kidneys and liver (if bound with other elements). When people are unable to remove arsenic quickly enough, spill over sites are hair, skin and nails followed by adipose (fatty) tissue. Could it be that being of slender build leaves this group limited tissue area for detoxification, allowing spillover in to the brain? Is there a greater propensity for outdoor activities in this group of people meaning they are more exposed than those with more fat stores?
The average age of onset of the various diseases seems to also have a bearing on rapidity of progression. ALS/MND and CJD seem to affect people from the ages of 40 and 45 respectively, whereas Parkinson’s and Alzheimer’s from 60 and 65 respectively. Is the rate of progression connected to age related trends in outdoor activity and therefore to exposure?
Thanks to Seb for the crucial exchanges required to get this information down on paper and thank you to Emergency News Channel and Twitter people for sharing their personal stories. Not only can we now see the mechanisms for brain alterations by arsenic, but also how it may affect other proteins in the body promoting illness.



Ageing is the main risk factor for Alzheimer’s disease and aluminium accumulates in human brain tissue with ageing.
Environmental or occupational exposure to aluminium results in higher levels of aluminium in human brain tissue and an early onset form of sporadic Alzheimer’s disease.
The genetic predispositions which are used to define familial or early-onset Alzheimer’s disease also predispose individuals to higher levels of brain aluminium at a much younger age.
Aluminium is accepted as a known neurotoxin, for example being the cause of dialysis encephalopathy, and its accumulation in human brain tissue at any age can only contribute to any ongoing disease state or toxicity.
Fascinating, thank you. What do you mean by "gain of function mechanism" or was this just a direct quote from the article? If you are right where is the arsenic coming from? Might there be a connection with Seb's insight into excess cremations?